March is Endometriosis Awareness Month; naturally, it is a good time to discuss myofascial pain related to endometriosis. We know that endometriosis can be extremely painful for women. Often, the referred symptoms are more bothersome than the diseased tissue itself. There is a poor correlation between pain severity and disease progression in endometriosis (Kor et al., 2020). Pain in endometriosis is frequently associated with myofascial trigger points (TrPs) in the abdomen, hips, and pelvic floor due to a phenomenon known as viscero-somatic convergence. Viscero-somatic convergence implies that shared somatic and visceral inputs to the spinal cord manifest visceral dysfunction as somatic pain (Aredo et al., 2017), which may include myofascial pain.
While physical therapy can not address the specific tissue impairments associated with endometriosis, physical therapists are well-equipped to improve pain levels and quality of life by treating the associated myofascial pain. Endometriosis and TrPs in the abdominal muscles are closely interconnected (Jarrell, 2011). A physical therapist trained in pelvic and abdominal health is integral to the healthcare team as it relates to women with endometriosis. Advanced training in the management of myofascial pain is critical with this patient population.
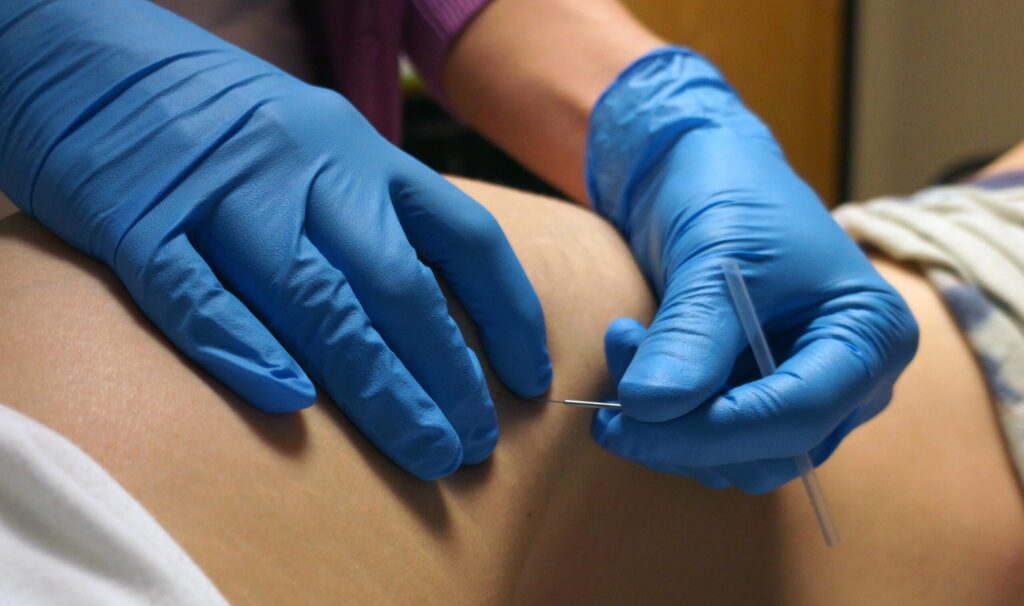
 Although only a few studies have examined the role of TrP dry needling in the management of endometriosis-related pelvic and abdominal pain, it would make sense that this intervention can be effective in treating the sequelae of this disease. Indeed, one study showed that dry needling can be beneficial in treating abdominal pain of unknown origin (Rajkannan & Vijayaraghavan, 2019). The European Association of Urology Guidelines Panel on Chronic Pelvic Pain confirmed a high prevalence of a myofascial pain component in chronic pelvic pain and recommended that myofascial pain must always be treated (Abreu-Mendes et al., 2023). A recent systematic review and meta-analysis of acupuncture for endometriosis concluded that acupuncture may also reduce the severity of menstrual pain and overall pelvic pain (Giese et al., 2023). Subjectively, patients report reduced pain and improved quality of life following regular dry needling of TrPs in the abdominopelvic region with endometriosis. Furthermore, as endometriosis is a chronic condition, the addition of TrP dry needling is a benefit to the patient, who may not desire repeated intra-vaginal treatments to address her myofascial pain.
Although only a few studies have examined the role of TrP dry needling in the management of endometriosis-related pelvic and abdominal pain, it would make sense that this intervention can be effective in treating the sequelae of this disease. Indeed, one study showed that dry needling can be beneficial in treating abdominal pain of unknown origin (Rajkannan & Vijayaraghavan, 2019). The European Association of Urology Guidelines Panel on Chronic Pelvic Pain confirmed a high prevalence of a myofascial pain component in chronic pelvic pain and recommended that myofascial pain must always be treated (Abreu-Mendes et al., 2023). A recent systematic review and meta-analysis of acupuncture for endometriosis concluded that acupuncture may also reduce the severity of menstrual pain and overall pelvic pain (Giese et al., 2023). Subjectively, patients report reduced pain and improved quality of life following regular dry needling of TrPs in the abdominopelvic region with endometriosis. Furthermore, as endometriosis is a chronic condition, the addition of TrP dry needling is a benefit to the patient, who may not desire repeated intra-vaginal treatments to address her myofascial pain.
Bottom line: women with endometriosis should not have to live with pain. Treating TrPs helps reduce pain, allowing these women to improve their daily function and overall quality of life. Trigger point dry needling is an effective tool to address the widespread TrPs associated with endometriosis.
Want to learn more about using dry needling for the management of endometriosis and other pelvic pain conditions? We’d love to see you at one of our Dry Needling for Pelvic Pain courses this spring!
The Obvious Choice for Dry Needling Education
Much More Than Just Dry Needling

The Dry Needling 1 course is an excellent starting point for learning the fundamentals of dry needling therapy. With a focus on the safe and effective application of dry needling techniques, you will gain a solid understanding of myofascial trigger points, needling techniques, precautions, and how to apply these techniques in clinical practice.
The 3-day Dry Needling for Pelvic Pain course is designed with the pelvic health practitioner in mind. We value the unique skill set of pelvic floor clinicians. We are proud to offer a dry needling course that features internal palpation and the effective dry needling treatment of internal pelvic floor muscles. The course will introduce the concepts of trigger point dry needling as it relates to the muscles of the pelvis and perineum. The course will integrate pain science research with anatomy and biomechanics of the pelvis and pelvic floor.

The 1+2-day Men’s Health Physical Therapy hybrid course will focus on assessing and managing the Men’s Health PT patient. It will include a detailed history-taking of the complex conditions men with pelvic dysfunction present with, such as male pelvic pain, male athletic pelvic pain, hard flaccid syndrome, post-prostatectomy urinary incontinence, and post-prostatectomy erectile dysfunction. This course will also address the challenges of setting up or building a men’s health PT service.
References
Abreu-Mendes, P., Baranowski, A. P., Berghmans, B., Borovicka, J., Cottrell, A. M., Dinis-Oliveira, P., Elneil, S., Hughes, J., Messelink, B. E. J., Tidman, V., Pinto, R., Tornic, J., Flink, I., Parsons, B. A., Zumstein, V., & Engeler, D. S. (2023). Myofascial Pelvic Pain: Best Orientation and Clinical Practice. Position of the European Association of Urology Guidelines Panel on Chronic Pelvic Pain. Eur Urol Focus, 9(1), 172-177. https://doi.org/10.1016/j.euf.2022.07.007
Aredo, J. V., Heyrana, K. J., Karp, B. I., Shah, J. P., & Stratton, P. (2017). Relating Chronic Pelvic Pain and Endometriosis to Signs of Sensitization and Myofascial Pain and Dysfunction. Seminars in Reproductive Medicine, 35(1), 88–97. https://doi.org/10.1055/s-0036-1597123
Giese, N., Kwon, K. K., & Armour, M. (2023). Acupuncture for endometriosis: A systematic review and meta-analysis. Integrative Medicine Research, 12(4), 101003. https://doi.org/https://doi.org/10.1016/j.imr.2023.101003
Jarrell, J. (2011). Endometriosis and abdominal myofascial pain in adults and adolescents. Current Pain and Headache Reports, 15(5), 368-376. https://doi.org/10.1007/s11916-011-0218-y
Kor E, Mostafavi S, Mazhin Z, Dadkhah A, Kor A, Arvanagh SH, Noroozi SG, Sadri G. Relationship between the severity of endometriosis symptoms (dyspareunia, dysmenorrhea and chronic pelvic pain) and the spread of the disease on ultrasound. BMC Res Notes (2020). 13:546.
Rajkannan, P., & Vijayaraghavan, R. (2019). Dry needling in chronic abdominal wall pain of uncertain origin. Journal of Bodywork and Movement Therapies, 23(1), 94-98. https://doi.org/https://doi.org/10.1016/j.jbmt.2018.01.004